The Primary Goal of Pain Management
The main objective is generally not total pain eradication (which is often unrealistic for chronic conditions), but rather achieving a level of pain control that allows the patient to
- Restore function and mobility.
- Improve sleep and mood.
- Maintain independence.
- Live a fulfilling life even in the presence of some residual pain.
Key Components of a Comprehensive Pain Plan
Pain management utilizes a broad range of evidence-based strategies, categorized into the following core areas:
1. Physical and Rehabilitative Therapies
These are often considered first-line treatments, especially for chronic musculoskeletal pain, as they focus on long-term physical improvement.
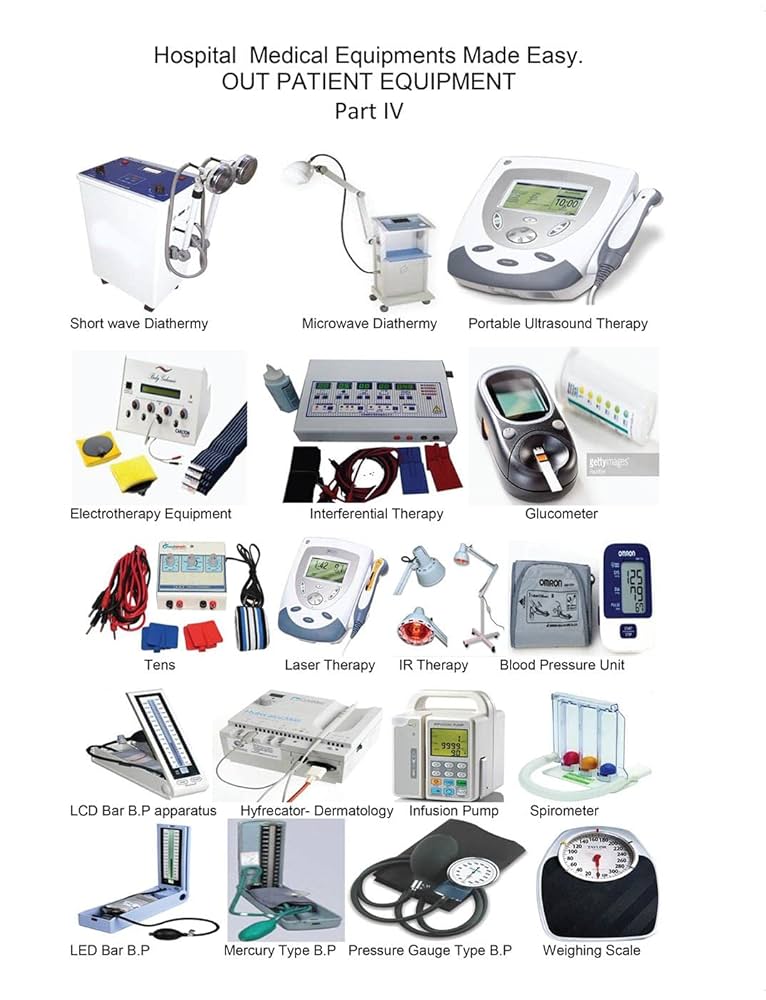
- Physiotherapy (Physical Therapy): Uses therapeutic exercise, manual therapy (mobilization, massage), and modalities (heat, cold, TENS) to improve strength, flexibility, posture, and movement mechanics.
- Occupational Therapy: Helps patients adapt daily tasks and environments to minimize pain and maximize independence.
- Exercise: Regular, paced activity (like walking or swimming) to improve overall fitness, which can reduce pain signals over time.
2. Pharmacological Treatments (Medication)
Medications are used to interrupt pain signals and reduce inflammation. These are carefully managed to minimize risks and side effects.
- Non-Opioids: Over-the-counter and prescription pain relievers like Acetaminophen and NSAIDs (Non-Steroidal Anti-Inflammatory Drugs)
- Adjuvant Analgesics: Medications originally developed for other conditions that also relieve pain, such as certain antidepressants (which help change how the brain processes pain) and anti-seizure drugs (for nerve pain).
- Opioids: Reserved for severe acute pain or pain from advanced illness, and managed under strict protocols due to the risk of dependence.
3. Interventional Procedures
These minimally invasive techniques are performed by pain specialists (often guided by imaging like X-ray or ultrasound) to directly target the source of pain.
- Injections: Such as Epidural Steroid Injections to reduce spinal nerve root inflammation, or Facet Joint Injections to treat joint pain in the spine.
- Nerve Blocks: Injecting local anesthetics around a nerve to interrupt pain signals.
- Radiofrequency Ablation (RFA): Using heat generated by radio waves to temporarily disable nerves responsible for sending pain signals.
- Implantable Devices: Including Spinal Cord Stimulators (which send mild electrical pulses to block pain signals) or Pain Pumps (which deliver medication directly to the spinal fluid).
4. Psychological and Self-Management Strategies
The emotional and mental toll of pain can intensify the physical experience.
Psychological support is vital, particularly for chronic pain.
- Cognitive Behavioral Therapy (CBT): Helps patients identify and change unhealthy emotions, thoughts, and behaviors related to pain, focusing on coping skills.
- Mindfulness and Relaxation: Techniques like deep breathing, meditation, and biofeedback to reduce stress and muscle tension, which often exacerbates pain.
- Pacing: Learning to balance activity with rest to avoid pain flare-ups and maintain consistent function.
- Goal Setting: Shifting focus from pain intensity to achievable, functional goals (e.g., walking for 30 minutes, doing house chores).
By combining these different strategies, pain management aims to treat not just the pain itself, but the whole person, facilitating a return to a richer, more active life.